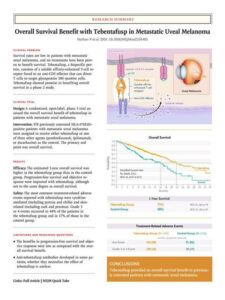
Author(s): Paul Nathan, M.D., Ph.D., Jessica C. Hassel, M.D., Piotr Rutkowski, M.D., Ph.D., Jean-Francois Baurain, M.D., Ph.D., Marcus O. Butler, M.D., Max Schlaak, M.D., Ryan J. Sullivan, M.D., Sebastian Ochsenreither, M.D., Reinhard Dummer, M.D., John M. Kirkwood, M.D., Anthony M. Joshua, M.D., Ph.D., Joseph J. Sacco, M.D., Ph.D., et al., for the IMCgp100-202 Investigators*
Author Affiliations
From Mount Vernon Cancer Centre, Northwood (P.N.), the Clatterbridge Cancer Centre NHS Foundation Trust, Wirral (J.J.S.), the University of Liverpool, Liverpool (J.J.S.), and Immunocore, Abingdon (S.E.A., C.H., H.G.) — all in the United Kingdom; the Department of Dermatology and the National Center for Tumor Diseases, University Hospital Heidelberg, Heidelberg (J.C.H.), the Department of Dermatology and Allergy, University Hospital, Ludwig Maximilian University of Munich, Munich (M.S.), the Department of Hematology and Oncology, Charité–Comprehensive Cancer Center (S.O.), Berlin, and the Department of Dermatology and the Center for Integrated Oncology, University Hospital Cologne, Cologne (C.M.) — all in Germany; Maria Sklodowska-Curie National Research Institute of Oncology, Warsaw, Poland (P.R.); Institut Roi Albert II des Cliniques Universitaires Saint-Luc and Université Catholique de Louvain, Brussels (J.-F.B.); Princess Margaret Cancer Centre, Toronto (M.O.B.); Massachusetts General Hospital Cancer Center, Boston (R.J.S.); the Department of Dermatology, University Hospital of Zurich, Zurich, Switzerland (R.D.); Hillman Cancer Center, University of Pittsburgh Medical Center, Pittsburgh (J.M.K.); Sidney Kimmel Cancer Center, Thomas Jefferson University Hospital, Philadelphia (M.O.); Kinghorn Cancer Centre, Saint Vincent’s Hospital, Darlinghurst, NSW, Australia (A.M.J.); Memorial Sloan Kettering Cancer Center (A.N.S.) and Irving Medical Center, Columbia University (R.D.C.) — both in New York; Institut d’Investigació Biomèdica de Bellvitge–Centro de Investigación Biomédica en Red de Oncología, Institut Català d’Oncologia, Barcelona (J.M.P.); University of Iowa Hospitals and Clinics, Iowa City (M.M.); Duke University, Durham, NC (A.K.S.S.); Earle A. Chiles Research Institute, Providence Cancer Institute, Portland, OR (B.C.); N.N. Blokhin Cancer Research Center, Moscow (L.D.); Centre Antoine Lacassagne, Nice (L.G.) and Institut Curie, Paris Sciences and Letters Research University, Paris (S.P.-N.) — both in France; Winship Cancer Institute, Emory University, Atlanta (M.Y.); and the Angeles Clinic and Research Institute, a Cedars–Sinai Affiliate, Los Angeles (O.H.).